Postural Photography in Concussion Assessment
Posted by Renee North, CPT, CPEP on 25th Sep 2025
Integrating Postural Grid Photography in Concussion Assessment: A Comprehensive Approach to Balance and Stability Screening
Concussion assessment has evolved significantly over the past decades, moving from subjective symptom reporting to objective, multi-modal evaluation protocols. While traditional balance testing methods like the Balance Error Scoring System (BESS) have provided valuable insights into postural stability deficits following brain injury, the integration of visual documentation through postural grid photography represents a logical advancement in comprehensive concussion care. This approach combines the established science of balance assessment with precise visual documentation, creating a more robust framework for baseline establishment, acute injury evaluation, and recovery monitoring.

The Scientific Foundation of Postural Assessment in Concussion
The relationship between brain injury and postural control is well-established in the literature. Concussion affects the complex neural networks responsible for maintaining balance, including the vestibular, visual, and somatosensory systems. These deficits manifest as observable changes in postural stability that can persist even after other symptoms resolve.
The Balance Error Scoring System, developed specifically for mild head injury populations, has been the gold standard for postural stability assessment in sports medicine. The BESS protocol evaluates six conditions—double leg stance, single leg stance, and tandem stance on both firm and foam surfaces—each performed barefoot with eyes closed for 20 seconds. Research has demonstrated that the BESS can effectively detect balance deficits in concussed individuals and track recovery patterns, with most athletes returning to baseline postural stability within 3-5 days post-injury.
More sophisticated assessment tools, such as the Sensory Organization Test (SOT) using force plate technology, provide additional objective data by measuring center of pressure movements and postural sway patterns. These systems systematically challenge different sensory inputs to identify specific deficits in the patient's ability to integrate somatosensory, visual, and vestibular information for postural control.
The Logic Behind Postural Grid Photography Integration
While functional balance tests like the BESS provide valuable kinetic data, they capture only a moment in time and rely heavily on examiner observation and scoring. The integration of postural grid photography addresses several limitations in current assessment protocols:
Objective Documentation: Static postural alignment can reveal compensatory patterns and asymmetries that may not be apparent during dynamic balance testing. These subtle changes in standing posture may persist longer than functional balance deficits and could indicate ongoing neurological compensation.
Baseline Establishment: Pre-injury postural photographs provide an individualized reference point that accounts for pre-existing postural variations, making post-injury comparisons more meaningful than population-based norms alone.
Longitudinal Tracking: Serial photography allows for precise documentation of postural changes throughout the recovery process, potentially identifying patterns that correlate with other recovery markers.
Enhanced Communication: Visual documentation facilitates communication between healthcare providers, coaches, parents, and athletes, providing a clear, objective record of postural status.
Implementing Postural Grid Photography in Clinical Practice
Equipment and Setup
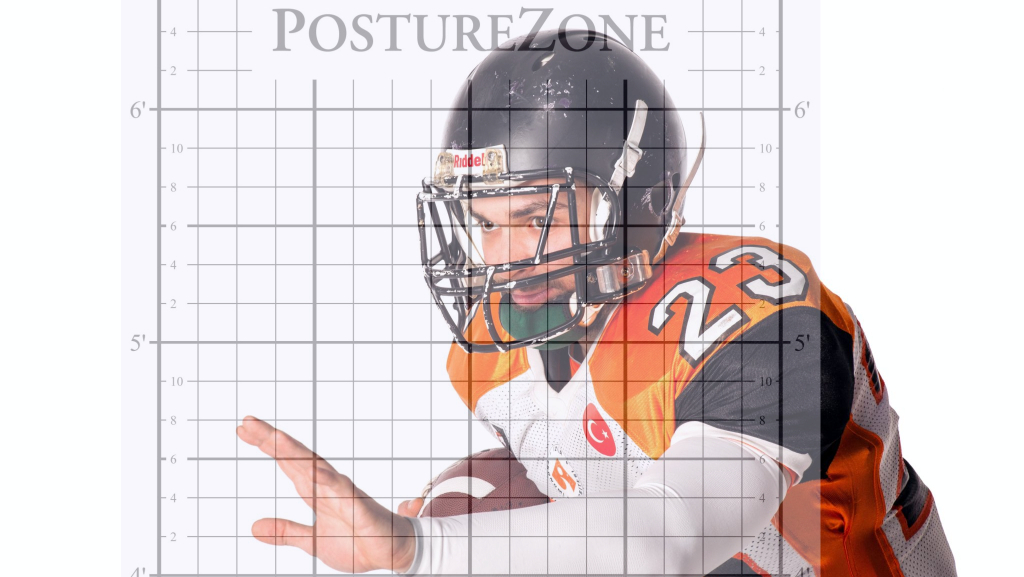
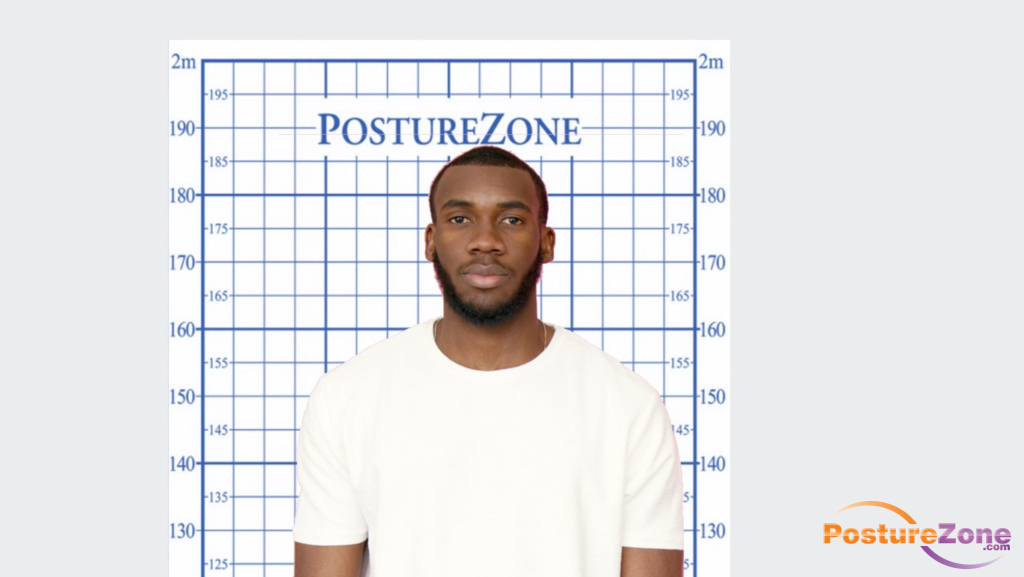
The postural grid system requires minimal equipment: a standardized grid background (typically 4-inch squares), a digital camera or smartphone with consistent positioning, and adequate lighting. The grid should be positioned to allow full-body visualization from multiple angles, with the patient standing at a standardized distance.
Standardized Photography Protocol
Baseline Documentation: Ideally captured during pre-season screening or initial evaluation, baseline images should include anterior, posterior, and lateral views. The patient should stand in a relaxed, natural position with arms at their sides, looking straight ahead.
Post-Injury Assessment: Following the same protocol used for baseline imaging ensures consistency. Photography should be performed as part of the comprehensive concussion evaluation, alongside traditional balance testing and cognitive assessment.
Recovery Monitoring: Serial imaging at predetermined intervals (typically at 24-48 hours, one week, and clearance examination) allows for systematic tracking of postural recovery patterns.
Integration with Traditional Balance Testing
The postural grid photography protocol should complement, not replace, established balance assessment tools. The logical sequence involves:
- Static Postural Photography: Documenting baseline postural alignment
- BESS Testing: Evaluating functional balance and postural stability
- Advanced Testing (when available): Force plate analysis or computerized dynamic posturography
- Comparative Analysis: Correlating static postural changes with functional balance deficits
Clinical Applications and Best Practices
Acute Injury Management
In the acute post-injury phase, postural grid photography can reveal immediate compensatory patterns that may not be apparent through functional testing alone. Subtle head tilts, shoulder asymmetries, or weight-bearing preferences captured in static imaging may indicate vestibular dysfunction or other neurological compensation mechanisms.
Return-to-Play Decision Making
The integration of postural photography into return-to-play protocols provides an additional objective measure of recovery. While an athlete may demonstrate normal BESS scores and report symptom resolution, persistent postural asymmetries visible on grid photography may indicate incomplete recovery and warrant continued monitoring.
Long-term Monitoring
Some individuals may develop persistent postural adaptations following concussion. Regular postural assessment through standardized photography can identify these patterns early, facilitating appropriate intervention and preventing secondary complications.
Evidence-Based Rationale
The integration of postural grid photography aligns with current evidence demonstrating that postural control deficits can persist beyond subjective symptom resolution. Research indicates that while most concussed athletes return to baseline postural stability within 3-5 days on functional tests, subtle static postural changes may persist longer. This disconnect between functional recovery and postural alignment suggests that comprehensive assessment should include both dynamic and static components.
Furthermore, the visual nature of postural assessment addresses the growing recognition that concussion recovery is highly individualized. By establishing patient-specific baselines and tracking individual recovery patterns, healthcare providers can make more informed decisions about treatment progression and activity clearance.
Implementation Considerations
Training and Standardization
Healthcare providers implementing postural grid photography should establish standardized protocols for patient positioning, camera placement, and image analysis. Consistency in technique is crucial for meaningful comparison between baseline and post-injury images.
Documentation and Legal Considerations
Postural photographs become part of the medical record and should be handled according to institutional privacy and documentation policies. Proper consent procedures and secure storage systems are essential components of any photography protocol.
Cost-Effectiveness
The minimal equipment requirements and ability to use standard digital photography make postural grid assessment highly cost-effective compared to advanced balance testing equipment. This accessibility makes the technique particularly suitable for smaller clinics, schools, and sports programs with limited resources.
Future Directions
The integration of postural grid photography represents an evolutionary step in concussion assessment, but future developments may include digital analysis tools for automated postural measurement, integration with wearable technology for continuous monitoring, and correlation studies linking static postural changes with long-term outcomes.
Advanced image analysis software could potentially quantify postural deviations with greater precision than visual assessment alone, while machine learning algorithms might identify subtle patterns predictive of recovery trajectory or risk of persistent symptoms.
Evolving Integrated Approach
The integration of postural grid photography into comprehensive concussion assessment protocols represents a logical advancement in evidence-based care. By combining the established science of balance testing with objective visual documentation, healthcare providers can enhance their ability to detect injury, monitor recovery, and make informed return-to-activity decisions.
This approach acknowledges that postural control is a complex, multi-faceted function that requires comprehensive assessment. While traditional tools like the BESS and SOT provide valuable functional data, the addition of static postural documentation creates a more complete picture of the patient's neurological status and recovery trajectory.
As concussion care continues to evolve toward more individualized, evidence-based approaches, the integration of multiple assessment modalities becomes increasingly important. Postural grid photography, when properly implemented and integrated with established assessment tools, provides healthcare providers with an additional objective measure to guide clinical decision-making and optimize patient outcomes.
The minimal cost, ease of implementation, and potential for enhanced assessment accuracy make postural grid photography a valuable addition to any comprehensive concussion management program. As we continue to refine our understanding of concussion pathophysiology and recovery patterns, visual documentation of postural status will likely become a standard component of best-practice concussion care.