Posture as an Emotional Health Indicator - Mental Health Evals
Posted by Steven Weiniger, DC, DIANM, CPEP on 3rd Oct 2025
Posture as an Emotional Health Indicator: Why Mental Health Practitioners Should Include Postural Assessment
The Hidden Connection Between How We Stand and How We Feel
Recent research is revealing what many practitioners have long suspected: the way we hold our bodies profoundly impacts our emotional state, and vice versa. A growing body of evidence suggests that adopting an upright posture can boost positive feelings and energy, while a slumped posture has detrimental effects on mood and can induce negative feelings and memories.
For mental health practitioners, this presents both an opportunity and a responsibility. While we've traditionally focused on cognitive and behavioral assessments, emerging research indicates that slouched shoulders and closed posture can indicate sadness or defeat, while open and active body language can show happiness or confidence.
The Science Behind Embodied Emotions
The connection between posture and emotion isn't just observational—it's neurologically grounded. Experimental research has confirmed that bodily postures can have a direct effect on emotional processing, with people adopting straight postures being faster at retrieving positive autobiographical memories.
Recent studies demonstrate that a wide variety of emotions differing in valence and arousal can be measured using body posture, making postural assessment a potentially valuable tool for practitioners working with clients across age groups.
Why Postural Assessment Matters in Mental Health Practice
1. Early Detection of Emotional Distress
Postural changes often precede or accompany emotional shifts. Clients may unconsciously adopt protective postures during periods of depression, anxiety, or trauma. By incorporating postural screening, practitioners can identify these physical manifestations early in treatment.
2. Comprehensive Treatment Planning
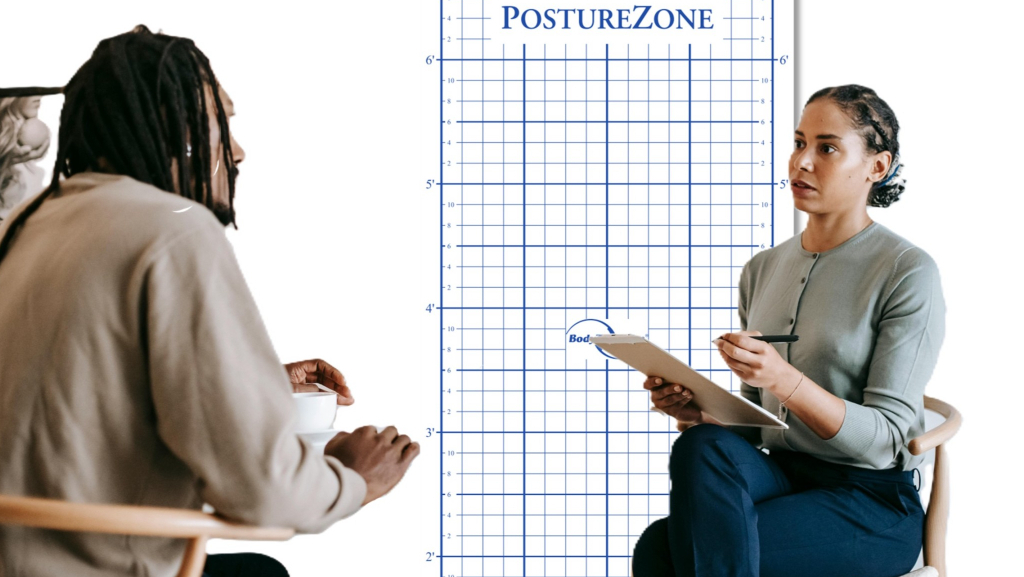
Understanding a client's postural patterns provides insight into how their emotional state manifests physically. This can inform both therapeutic interventions and referrals to complementary practitioners like physical therapists or chiropractors.
3. Treatment Progress Monitoring
Changes in posture can serve as objective indicators of therapeutic progress. As clients develop better emotional regulation, their postural patterns often improve correspondingly.
4. Client Awareness and Empowerment
Many clients are unaware of their postural habits. Simple awareness can be therapeutic, giving clients a concrete way to influence their emotional state through body positioning.
Implementing Postural Screening in Your Practice
Initial Assessment Protocol
Visual Observation Checklist:
With client standing in front of a posture grid
- Head position (forward head posture, tilting)
- Shoulder alignment (elevated, rolled forward, uneven)
- Spinal curves (excessive kyphosis, loss of lumbar lordosis)
- Pelvic position (anterior/posterior tilt)
- Weight distribution (favoring one side)
- Overall body openness vs. protective positioning
Simple Documentation:
- Use smartphone photography for baseline documentation
- Note correlations between postural findings and presenting emotional concerns
- Track changes over time alongside therapeutic progress
Integration with Mental Health Assessment
During Initial Intake:
- Include postural observation as part of mental status examination
- Ask clients about body awareness and physical tension patterns
- Note any client reports of chronic pain or physical discomfort
Ongoing Sessions:
- Begin sessions with brief posture check-ins
- Use postural cues as discussion points for emotional exploration
- Incorporate simple postural exercises as homework between sessions
Technology Tools for Modern Practitioners
Modern postural assessment doesn't require extensive training or expensive equipment. Simply taking a photograph of the client standing in front of a postural grid using any mobile device, tablet, or camera provides the current gold standard for objective postural documentation and analysis.
These tools can:
- Provide objective measurements for progress tracking
- Included with reports for interdisciplinary care coordination
- Offer visual feedback that motivates clients because it's easy to understand
- Create baseline documentation for insurance and treatment planning
The Interdisciplinary Approach
Recognizing the posture-emotion connection opens doors for collaborative care. Mental health practitioners can:
- Partner with physical therapists for comprehensive treatment approaches
- Refer to CPEP® postural specialists when structural issues are identified
- Collaborate with yoga therapists or movement specialists
- Work with occupational therapists for ergonomic interventions
Case Study Applications
Anxiety Disorders: Clients with anxiety often display protective postures—rounded shoulders, collapsed chest, forward head position. Addressing these patterns can complement traditional anxiety treatments.
Depression: The characteristic "slumped" posture of depression isn't just a symptom—it may perpetuate the emotional state. Postural interventions can be integrated with cognitive-behavioral approaches.
Trauma: Trauma survivors often develop protective postural patterns. Understanding these can inform trauma-sensitive treatment approaches and somatic interventions.
Getting Started: A Practical Framework
Week 1-2: Observation Phase
- Begin noting postural patterns in current clients
- Document correlations between posture and emotional presentations
- Practice visual assessment skills using a posture grid
Week 3-4: Integration Phase
- Introduce simple postural awareness exercises
- Begin using posture as a therapeutic topic
- Consider technology tools for more objective assessment
Month 2+: Collaboration Phase
- Develop referral relationships with movement professionals
- Create integrated treatment plans incorporating postural elements
- Track outcomes combining traditional metrics with postural changes
The Future of Integrated Care
As our understanding of embodied cognition grows, the integration of postural assessment into mental health practice represents a natural evolution toward more comprehensive care. Practitioners are increasingly using observations of posture and facial expressions as part of behavioral assessments, recognizing that emotional health and physical presentation are intimately connected.
By incorporating postural screening into initial evaluations, mental health practitioners can:
- Provide more comprehensive assessments
- Offer clients additional tools for self-regulation
- Enhance treatment effectiveness through embodied interventions
- Build stronger interdisciplinary relationships
- Position their practice at the forefront of integrative mental health care
Conclusion
The research is clear: posture and emotion are interconnected in ways that can inform better mental health treatment. By adding simple postural assessment to your practice toolkit, you're not just staying current with research—you're providing your clients with a more complete understanding of their emotional health and additional pathways to healing.
The integration of postural screening represents a low-cost, high-impact addition to mental health practice that honors both the complexity of human experience and the practical needs of modern healthcare delivery.
Ready to integrate postural assessment into your practice? Explore professional training opportunities and assessment tools at PostureZone.com, where mental health meets structural health for comprehensive client care.